Cancer Blog
BLOG
Article Categories
Prostate Cancer
Prostate cancer is the second most common cancer in men worldwide. Screening for prostate-specific antigen (P.S.A.) levels have led to prostate cancer being increasingly diagnosed.
Common symptoms of prostate cancer are difficulty urinating, reduced stream of urine, blood in the semen, erectile dysfunction and discomfort in the pelvic area.
The initial treatment options for patients with non-metastatic prostate cancer (cancer that has not spread beyond the primary site to other areas in the body) consists of active surveillance, radical prostatectomy and radiotherapy. The choice of treatment is determined by clinical staging (progression of disease), the P.S.A. level, Gleason score, patient preference, life expectancy, patient functional status and resource availability1-3.
What is Prostate Brachytherapy?
Prostate brachytherapy is a form of internal radiation therapy used to treat prostate cancer. It’s an established and effective cancer treatment, and involves placing temporary or permanent radioactive sources into the prostate tissue. This allows high doses of radiation to be delivered to the cancer cells, within the prostate gland, whilst reducing radiation of normal tissues.
A major advantage of brachytherapy is that it can be completed within 1-2 days with little time lost from normal activities. Depending on the risk category of the patient, it can be used alone or in combination with external beam radiotherapy. New developments in prostate brachytherapy include its use in salvage treatment, following relapse in patients who received prior radiotherapy and as a boost to permit dose escalation 2;4.
How is it performed?
The patient undergoes general or spinal anaesthesia. Radiation sources are then placed in the prostate under rectal ultrasound guidance. Low-dose rate brachytherapy (L.D.R.) is delivered through a vessel known as ‘’seeds’’ and is permanent; whilst high-dose rate brachytherapy (HDR) is delivered with hollow catheters and is temporary.
What are the side effects?
Anatomically the prostate gland is close to the urethra, bladder and rectum. These structures can develop acute and late side effects from prostate brachytherapy. Most commonly, there can be worsening of urinary symptoms, such as increased frequency, nocturia (frequent urination at night), urination hesitancy, urgency or a weak urinary stream and urinary retention. Uncommon complications are urethral strictures, rectal bleeding, rectal fistulas and erectile dysfunction 2;5.
Which patients should not have bracytherapy?
Patients with the following considerations may not be recommended for this type of treatment:
• Limited lifespan
• Unacceptable operative risks
• International prostate symptom score (IPSS) score >20
• Transurethral resection of the prostate (TURP) within 3-6 months
• Rectal fistula
• Pubic arch interference
What can be expected after the procedure?
Patients may experience mild discomfort and swelling in the perineum where the needles were placed. Ice packs and analgesia may be used for alleviation of discomfort. Patients should avoid strenuous activities that may irritate the perineum, like bike riding and running. Follow-up PSA testing will be ordered by your radiation oncologist.
The take home message:
Prostate brachytherapy is a cost effective, convenient radiation technique with excellent oncologic outcomes that is recommended for the curative treatment of men with prostate cancer.
Author: Dr Nirsha Chiranjan - Radiation Oncologist at DMO.
REFERENCES
1. National Comprehensive Cancer Network (NCCN). NCCN Clinical practice guidelines in oncology.
2. THE GEC ESTRO HANDBOOK OF BRACHYTHERAPY
3. Bekelman JE, Rumble RB, Chen RC, et al. Clinically Localized Prostate Cancer: ASCO Clinical Practice Guideline Endorsement of an American Urological Association/American Society for Radiation Oncology/Society of Urologic Oncology Guideline. J. Clin Oncol 2018; :JCO1800606.
4. Chin J, Rumble RB, Kollmeier M, et al. Brachytherapy for patients with prostate cancer: American Society of Clinical Oncology/Cancer Care Ontario joint guideline update. J Clin Oncol 2017.
5. Keyes M, Miller S, Moravan V, et al. Predictive factors for acute and late urinary toxicity after permanent prostate brachytherapy: long-term outcome in 712 consecutive patients. Int J Radiat Oncol Biol Phys 2009; 73:1023.
What are gynaecological cancers?
Gynaecological Cancer Awareness Month aims to encourage more women to be aware of the signs and symptoms of the disease and preventive strategies. It is a month that encourages women to openly speak about their health without shame or embarrassment. It highlights the need for better sex education amongst both men and women.
Early detection can lead to effective treatment and a better prognosis.
Gynaecological cancers are malignancies that develop in a woman’s reproductive tract. These include cervical, ovarian, endometrial, vulvar and vaginal cancer.
Cervical and endometrial cancer are the two most common cancers affecting South African women.
Cervical cancer
The cervix is the tissue connecting the uterus to the vagina. 1 in 40 women in SA are affected by cervical cancer. It’s the second most common cancer affecting women in SA, after breast cancer. Cervical cancer kills at least eight women every day *1.
HPV
A common sexually transmitted virus, human papillomavirus (HPV), is the most common risk factor for cervical cancer.
There are many different strains of HPV but the development of cervical cancer is linked to high-risk strains identified as strains 16 and 18.
Signs and symptoms can include:
- Abnormal vaginal bleeding. It could be bleeding after menopause, bleeding after sex, or bleeding between periods.
- Vaginal discharge which could be copious, foul-smelling and be accompanied with pelvic pain.
- Abdomen pain and backache.
- In advanced disease, women may complain of poor appetite; weight loss; bone pain; swelling of one of the lower legs; loss of bowel and bladder control; blood in urine or stool *4.
Screening
Screening is in the form of co-testing, made up of Pap smears and HPV testing. The frequency in which women get Pap smears is not the same for everyone.
How often a woman needs a Pap smear depends on several factors, such as age, general health, and findings from previous Pap smears. Women are then placed into an average- or high-risk category.
The best way to detect precancerous changes and early cervical cancer is to have regular screening tests. Screening women for HPV is a very effective way of preventing cervical cancer. Women between the ages of 21 - 65 should have three to five yearly Pap smears, depending on risk category. Women between the ages of 25 - 65 should be tested for HPV as well (co-testing) *5,6,7.
We promote conversation between women and their Doctors to ensure that they understand their personal risk profile and how frequently they should screen.
Prevention
Get vaccinated
The HPV vaccine protects against the two strains of HPV that are responsible for 70 - 80% of cervical cancers. There are two vaccines available in South Africa. The bivalent vaccine is approved for both girls and boys from the age of nine and is available at most retail pharmacies and school-based vaccination programmes.
Lifestyle modification
Stop smoking. Smoking produces chemicals that may damage the cells of the cervix and make cancer more likely to develop. Quitting smoking or, better still, never starting, will reduce your risk.
Limit the number of sexual partners and practise safe sex to prevent HIV infection or sexually transmitted diseases. HIV positive women have a high prevalence of co-infection with HPV. If you are HIV positive, it is important to be compliant on HAART and have regular Pap smears.
Endometrial cancer
The endometrium is the tissue lining the inner cavity of the uterus. Endometrial Cancer, also known as uterine cancer, is the most common gynaecologic malignancy in developed countries and the second most common in developing countries.
Risk factors for this type of cancer include many variables such as age, unopposed oestrogen therapy, Tamoxifen therapy (less than 1% per year), a wide oestrogen window (early menstruation and late menopause), Nulliparity (a woman never having given birth), Polycystic ovarian syndrome, obesity, diabetes, Lynch syndrome, Cowden syndrome and a family history of breast, ovarian, colon, endometrial cancer *8
Signs and symptoms
- Abnormal uterine bleeding is the cardinal symptom of endometrial cancer.
- Incidental finding on imaging. A thickened endometrial lining is sometimes found incidentally on ultrasound, CT or MRI performed for another indication.
- Incidental finding at hysterectomy. Endometrial carcinoma or hyperplasia is sometimes discovered incidentally when hysterectomy is performed for benign disease.
Screening and prevention Routine screening of asymptomatic women is not advised. Lifestyle modification includes maintaining a healthy weight, exercising regularly and healthy diet may be preventative *9.
References:
- CANSA: nicd.ac.za
- Comparison of risk factors for invasive squamous cell carcinoma and adenocarcinoma of the cervix: collaborative reanalysis of individual data on 8,097 women with squamous cell carcinoma and 1,374 women with adenocarcinoma from 12 epidemiological studies.AU, International Collaboration of Epidemiological Studies of Cervical Cancer SO Int J Cancer. 2007;120(4):885.
- Human papillomavirus is a necessary cause of invasive cervical cancer worldwide.AUWalboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ, Muñoz N SO J Pathol. 1999;189(1):12.
- DiSaia PJ, Creasman WT. Invasive cervical cancer. In: Clinical Gynecologic Oncology, 7th ed., Mosby Elsevier, Philadelphia 2007. p.55.
- ACOG Committee Opinion No. 463: Cervical cancer in adolescents: screening, evaluation, and management. American College of Obstetricians and Gynecologists SO Obstet Gynecol. 2010;116(2 Pt 1):469.
- European Cervical Cancer Association. http://www.ecca.info/ (Accessed on December 16, 2014).
- Practice Bulletin No. 168: Cervical Cancer Screening and Prevention.Committee on Practice Bulletins—Gynecology SO Obstet Gynecol. 2016;128(4):e111.
- ACOG practice bulletin, clinical management guidelines for obstetrician-gynecologists, number 65, August 2005: management of endometrial cancer. American College of Obstetricians and Gynecologists Obstet Gynecol. 2005;106(2):413.
- UPTODATE
A cancer survivor refers to any person who has been diagnosed with cancer. Survivorship begins at the time of diagnosis and includes the periods of initial treatment with intent to cure, cancer-free survival, chronic or intermittent disease, and end of life care.
There are millions of survivors worldwide. This number is expected to grow due to improvements in cancer screening, increases in life expectancy following definitive cancer treatment and the aging of the population. For cancer survivors who are no longer in active treatment, health care needs include surveillance for recurrence, screening for the development of subsequent primary cancers, monitoring and intervention for the long-term and late physical and psychological effects of cancer and preventive care.
For some survivors, the consequences of cancer are minimal with many returning back to a normal life after treatment. However, many survivors experience physical and psychosocial effects of cancer and its treatment.
Risk of recurrence:
Following treatment of a primary cancer, survivors are at risk for recurrence. Recurrences may occur where the cancer was originally diagnosed or in a different location. The timing and patterns of recurrence, particularly of distant disease, vary by cancer type and stage at diagnosis. Patients with the highest risk of developing a second (subsequent) primary cancer includes survivors of head and neck cancers and Hodgkin lymphoma.
Subsequent primary cancers in cancer survivors occur due to multiple clinical factors, including prior treatment for the primary cancer (eg, chemotherapy, radiation therapy) lifestyle habits (eg, smoking, obesity) and genetic factors. This data suggests an opportunity for doctors to reduce or prevent the risk of subsequent primary cancers in cancer survivors through lifestyle interventions (eg, cease smoking, alcohol counselling, diet, and physical activity) as well as cancer screening and genetic counselling.
Monitoring for long-term effects of cancer and its treatment
Survivors are at risk for other conditions related to both their disease and its treatment, which are of increasing importance as cancer survival rates improve. Late physical effects of treatment may include pain, fatigue, depression, lymphoedema, urinary and bowel problems, cardiotoxicity, subsequent malignancy, peripheral neuropathy, hearing loss, infection, loss of bone mass, premature menopause in women and sexual dysfunction. Your Oncologist will advise you of the risks and side effects of treatment, as these vary between various treatment approaches.
Psychosocial well-being — Cancer survivors have been shown to experience a number of difficulties that can impact general quality of life, including depression, anxiety, fatigue, cognitive limitations, sleep problems, sexual dysfunction, pain, and opioid dependence.
A number of interventions for cancer survivors have been evaluated, with both psychosocial and exercise interventions reporting beneficial effects on quality of life.
Fertility and parenthood — Cancer therapy may put male and female survivors at risk for infertility. Patients may be concerned about their chances of getting pregnant, suffering a miscarriage, and/or achieving a successful pregnancy outcome. Furthermore, cancer survivors may be fearful that their history of cancer or its treatment will have an adverse impact on offspring conceived after their cancer treatment, such as placing them at risk for malignancy, congenital anomalies, or impaired growth and development. They may also be concerned about the risks of pregnancy on cancer recurrence. For these patients, education regarding reproductive function is an important aspect of their care.
Preventative Care
- Both diet and physical activity can improve the quality of life and can minimize both disease and treatment-related side effects in cancer survivors.
- Smoking — Cancer survivors are at increased risk for subsequent cancers, and the risks are significantly higher among those who continue to smoke.
- Limit alcohol consumption
- Genetic evaluation and testing-genetic factors may have important implications for the survivor's family members
Survivorship Care Plan:
Cancer survivorship is often a hard transition to a new normal. A cancer survivorship care plan is often formulated between the patient and treatment team. It is a record of your cancer and treatment history. It may list the follow up needed, future tests required, possible long-term side effects and preventative strategies.
Conclusion:
Cancer survivors want health, longevity and quality of life. The road to these outcomes is often riddled with obstacles involving medical uncertainty, treatment outcomes, social expectations and financial burden. An active relationship between Health Practitioners and Patients is important at all levels of care through the cancer journey.
The full referenced article is available on request.
By Dr Nirasha Chiranjan

Prostate and Testicular Cancer ft. Ismail Abrahams & Dr Ingo de Muelenaere: Listen Here
Please feel free to share the clip with all your freinds and family.
Stay aware of the latest information on the COVID-19 outbreak, available on the WHO website and through the South African government's Covid-19 portal at sacoronavirus.co.za. COVID-19 has affected most countries around the world, at the time of this publication with widespread transmission. Most people who become infected experience mild illness and recover, but it can be more severe for others.
Take care of your health and protect others by doing the following:
Wash your hands frequently
Regularly and thoroughly clean your hands with an alcohol-based hand rub or wash them with soap and water.
Why? Washing your hands with soap and water or using alcohol-based hand rub kills viruses that may be on your hands.
Maintain social distancing
Maintain at least 1 metre (3 feet) distance between yourself and other people. Avoid close contact with anyone who is coughing or sneezing.
Why? When someone coughs or sneezes they spray small liquid droplets from their nose or mouth which may contain virus. If you are too close, you can breathe in the droplets, including the COVID-19 virus if the person coughing has the disease.
Avoid touching eyes, nose and mouth
Why? Hands touch many surfaces and can pick up viruses. Once contaminated, hands can transfer the virus to your eyes, nose or mouth. From there, the virus can enter your body and can make you sick.
Practice respiratory hygiene
Make sure you, and the people around you, follow good respiratory hygiene. This means covering your mouth and nose with your bent elbow or tissue when you cough or sneeze. Then dispose of the used tissue immediately.
Why? Droplets spread virus. By following good respiratory hygiene you protect the people around you from viruses such as cold, flu and COVID-19.
If you a have fever, cough and difficulty breathing, seek medical care early
Stay home if you feel unwell. If you have a fever, cough and difficulty breathing, seek medical attention and call in advance. Follow the directions of your local health authority.
Why? National and local authorities will have the most up to date information on the situation in your area. Calling in advance will allow your health care provider to quickly direct you to the right health facility. This will also protect you and help prevent spread of viruses and other infections.
Stay informed and follow advice given by your healthcare provider
Stay informed on the latest developments about COVID-19. Follow advice given by your healthcare provider, your national and local public health authority or your employer on how to protect yourself and others from COVID-19.
Why? National and local authorities will have the most up to date information on whether COVID-19 is spreading in your area. They are best placed to advise on what people in your area should be doing to protect themselves.
Protection measures for persons who are in or have recently visited (past 14 days) areas where COVID-19 is spreading
- Follow the guidance outlined above.
- Stay at home if you begin to feel unwell, even with mild symptoms such as headache and slight runny nose, until you recover. Why? Avoiding contact with others and visits to medical facilities will allow these facilities to operate more effectively and help protect you and others from possible COVID-19 and other viruses.
- If you develop fever, cough and difficulty breathing, seek medical advice promptly as this may be due to a respiratory infection or other serious condition. Call in advance and tell your provider of any recent travel or contact with travelers. Why? Calling in advance will allow your health care provider to quickly direct you to the right health facility. This will also help to prevent possible spread of COVID-19 and other viruses.
At our DMO Cancer Care Centres, we have updated our Visitors Policy as well as implemented screening and pre-screening processes.
Please contact our centre prior to your appointment to ensure that you are aware of our updated procedures
With acknowledgement to the World Health Organisation for the information contained herein.
|
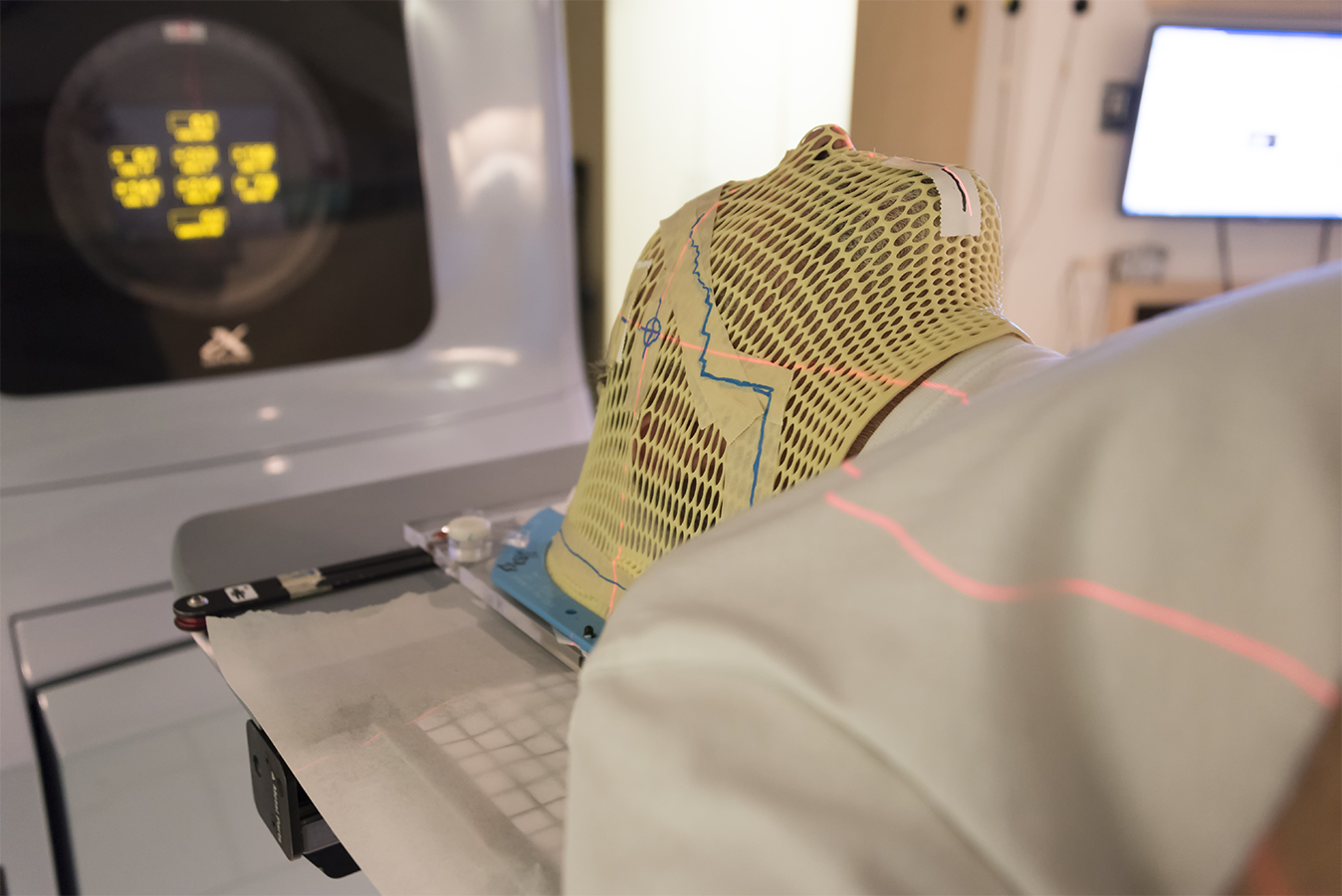
Cancer is a life journey. At Sandton Oncology, we don’t only manage an illness, we manage our patients’ overall well-being. Our goal is to treat patients with state of the art equipment and technologies. Our team provides patient focused care and services, which cover numerous aspects of the patient’s experience from diagnosis to treatment, follow up care and psycho social support – to enhance their lives throughout the journey.
Our new cancer centre of excellence, situated at 200 Rivonia Medical Centre, offers leading medical oncology and radiotherapy treatments. We have opened the centre, with a state of the art Versa HD Linear Accelerator that is capable of delivering complex radiotherapy treatments to the head and body with shorter treatment times, sparing more healthy tissue and thus decreasing side effects. Our 4D CT scanner for treatment planning will ensure high precision targeting of the tumour and decrease the risks of side effects of treatment. Image guided radiation therapy and gated radiation therapy is possible with the new technology available at the centre. Our Medical Oncology team offers leading global, evidence based systemic therapies with modern drugs in a safe and comfortable environment. With the added feature of a cancer focused research department, this allows us to offer patients the opportunity to participate in cutting edge clinical trials, at no cost, including covering transportation needs. Dr Keo Tabane adds: ‘’these clinical trials are available to both the insured and un-insured population, which allows us to make a meaningful impact across all communities’’.
Our Medical Oncology team consists of Dr K. Tabane; Dr S.W. Chan and Dr O. Ogude; who work closely with our team of Radiation Oncologists: Dr R. de Mûelenaere; Prof. B. Donde; Dr S. Naidoo; Dr N. Chiranjan and Dr Y. Mark. We actively participate in two leading multi-disciplinary team (M.D.T.) committees, covering Head and Neck Cancer and Breast Cancer. In the M.D.T. meetings, emphasis is on collaborative decision-making and treatment planning, where the core team members of relevant specialties participate to share their knowledge and make collective evidence-based recommendations for holistic patient care. This assures high quality treatment decisions by a panel of experts for the patient.
Our Oncologists are rostered on call
|
|
At DMO, we strive to keep our patients at the centre of what we do. Based on this vision, we looked at the patient care pathway and asked important questions related to patient need.
To ensure that we focused our services holistically to meet a wider range of patient care needs, through the cancer journey, we worked with prominent medical specialists to create a well-positioned space of collaboration, service and treatment excellence and care within a beautiful, modern setting.
Our collection of care teams that are focused on providing patient centred care, provide services which cover many aspects of the patient journey from diagnosis to treatment and follow up care.
Based on this understanding, we are very excited to announce the opening of our new location situated on 200 Rivonia Road, Morningside, in the greater Sandton area.
Breast Cancer Treatment
Services at the Centre will include a Female Radiology Centre, Diagnostic Radiology Department with CT scanners and MRI unit planned, Day Wards, Specialist Surgeons, Medical Aesthetics and Skin Renewal. A multi-modality solution for care journeys such as Breast Cancer Treatment.
Sandton Oncology will offer leading Medical Oncology and Radiotherapy Treatments with an advanced linear accelerator Versa HD, which will be capable of completing radiotherapy treatments such as Stereotactic Radiosurgery including body stereotaxis, Volumetric Modulated Arc Radiotherapy (VMAT) – which is a new proven type of Intensity-modulated radiation therapy (IMRT) technique.
The Versa HD is equipped with sophisticated conformal beam-shaping technology and High Dose rate mode delivery. Versa HD is designed to provide the precision and speed necessary to deliver advanced stereotactic radiotherapy (SRT) and stereotactic radiosurgery (SRS), techniques that demand the maximum accuracy in tumour targeting and protection of critical structures.
“Versatile, all-in-one system from classic radiotherapy to advanced stereotactic precision”
At the same time, Versa HD gives cancer management professionals the flexibility to employ conventional therapies to treat the broad spectrum of tumours throughout the body. Proven in its application, Versa HD is the only system to unlock the true potential of high dose rate delivery due to its market-leading leaf speeds and ultra-low leaf transmission.
In short, this means:
- Reduced treatment times with rapid leaf speeds and high dose delivery
- Provide the potential to deliver SBRT/SRS in a standard time slot which equals shorter treatment times for the patient
- Lower non-therapeutic doses to protect organs-at-risk and potentially reduce the risk of secondary cancer
- Exploit the full potential of high doses for advanced therapies
- Provide custom configurations for unique clinical needs
- Utilize the latest imaging technology to allow soft tissue visualization during treatment
Other patient amenities at the centre will include a Dischem pharmacy, coffee shop and restaurant.
We will be moving offices from 159 Rivonia Road on the 26th of October 2017 and will reopen on the 1st of November 2017 at 200 Rivonia Road.
Shaun-Anthony McPhail
28 September 2017
Achknowledgement: Elekta: Versa HD TM
Rectal Cancer
Surgical excision is considered to be essential for the curative treatment of rectal cancer, however, the addition of chemotherapy and radiotherapy in either the neoadjuvant or adjuvant setting play an important role in the treatment of locally advanced rectal cancer.
Neoadjuvant chemo-radiation is the preferred treatment in advanced rectal cancer, as per the results of the German Rectal Cancer Trial1. This trial compared pre-operative and post-operative CRT in patients with T3/T4 or node positive rectal cancer.
Although there was no difference in overall survival between the neo-adjuvant or adjuvant therapy groups, pre-operative therapy was associated with improved local control. The group that received pre-operative therapy had a local relapse rate of 6% versus the post-op group who had a local relapse rate of 13%. Post-operative complication rates were the similar in both groups.
Advantages and Disadvantages of Neoadjuvant Therapy in Rectal Cancer
Advantages:
- Improves resectability in locally advanced disease
- Reduces the risk of locoregional recurrence after surgery
- Reduces the risk of treatment associated toxicity. Treatment fields are often smaller especially for patients requiring AP resections.
- Irradiating tissue that is surgery naïve and thus better oxygenated may lead to greater radiotherapy sensitivity
- May increase chances of a sphincter sparing procedure in patients with a low lying tumour
- Can assess the tumours response to chemo-radiotherapy to help to tailor future therapies
Disadvantages:
- Possible over-treatment of patients with early stage disease or undetected metastases.
- Clinical staging using imaging and examination is less accurate then pathological staging. There is therefore a risk of over-treatment of disease that has been clinically over or under staged.
- The German Rectal Cancer Trial showed that 18% of patients staged by endo-rectal sonar as having T3 or node positive disease had node negative disease confined to the rectal wall on later pathological assessment1.
Rectal Cancer- Indications for Adjuvant Therapy
In cases where primary surgery has been performed, the following factors are indications for adjuvant therapy:
1) T3 disease – tumour extending through the muscularis propria into the perirectal tissue.
2) T4 disease- tumour penetrating the surface of the visceral peritoneum (T4a), tumour directly invading into or adherent to adjacent organs or structures (T4b).
3) Positive resection margins
4) Node positive disease.
In these cases, post-operative chemo-radiation has been shown in multiple phase III trials to be associated with improvements in both disease free and overall survival rates.2,3
Dr Yael Mark
28 September 2017
References:
- German Rectal Cancer Study Group, Sauer et al, 2004
- GITSG 7175 (Thomas and Lindblad, 1988)
- NCCTG 79-47-51 (NEJM 1991)
 Squamous carcinomas of the head and neck are often multiple, recurrent and aggressive. Surgery, radiotherapy and concurrent chemo-radiation are established standards of care in management of head and neck cancers. Locoregional failure is a major source of morbidity and mortality. Incidence can be as high as 50 % of all patients. [1,2] Field cancerization from chronic alcohol and tobacco usage results in second primary tumours at different sites with trimodality treatment often required. Local recurrences, nodal recurrences and second primary tumours represent part of the heterogeneity of this treatment population. New primary cancers should respond better to treatment than recurrent tumours in a previously irradiated field due to the inherent aggressiveness and radioresistance of recurrent tumour cells.
Squamous carcinomas of the head and neck are often multiple, recurrent and aggressive. Surgery, radiotherapy and concurrent chemo-radiation are established standards of care in management of head and neck cancers. Locoregional failure is a major source of morbidity and mortality. Incidence can be as high as 50 % of all patients. [1,2] Field cancerization from chronic alcohol and tobacco usage results in second primary tumours at different sites with trimodality treatment often required. Local recurrences, nodal recurrences and second primary tumours represent part of the heterogeneity of this treatment population. New primary cancers should respond better to treatment than recurrent tumours in a previously irradiated field due to the inherent aggressiveness and radioresistance of recurrent tumour cells.
Surgery, palliative chemotherapy and re-irradiation remain difficult salvage options due to patient medical co-morbidities; site and extent of tumours; secondary sequelae from previous treatments and patient preference. [3,4].
Re-irradiation can be delivered using external beam radiotherapy, brachytherapy or stereotactic radiosurgery. Severe adverse reactions in high dose irradiated areas have been well documented over the past decades. The use of modern radiotherapy techniques (intensity modulated radiation therapy (IMRT) and radiosurgery (SRS)) with its advanced precision technology has improved the outcome and quality of life of these patients.[5,6]
Brachytherapy is a term used to describe the short distance treatment of cancer with radiation from small, encapsulated radionuclide sources. This type of treatment is given by placing sources directly into or near the volume to be treated. The physical advantage of brachytherapy treatments compared with external beam radiotherapy is the improved localized delivery of dose to the target volume of interest. The disadvantage is that brachytherapy can only be used in cases in which the tumour is well localized and relatively small. Brachytherapy has achieved good local control in selected patients. Although brachytherapy has a potential to cure oral, oropharyngeal, nasopharyngeal, and lymph node recurrences [8], only superficial small tumours can be treated, and the number of experienced institutions is limited.
IMRT is an advanced form of three dimensional radiotherapy that not only conforms (high) dose to the target volume but also conforms (low) dose to sensitive structures. It is a radiation therapy technique in which non-uniform fluence is delivered to the patient through inverse planning. Benefits of IMRT are better normal tissue sparing resulting in reduced toxicity, higher doses to the target with a higher chance of cure and more dose within a fraction therefore fewer fractions. Studies have shown that IMRT is well tolerated and feasible in patients treated with previous radiotherapy for recurrent head and neck cancer. In some series it resulted in a better locoregional tumour control than conventional radiotherapy. [10]
Stereotactic radiosurgery and stereotactic radiotherapy allows highly conformal dose distribution and dose delivery to within a few mm for head and neck cancers. The practical advantage is a short duration of treatment usually lasting one day for radiosurgery and two weeks of alternative day treatment for stereotactic radiotherapy. Radiation doses are either single fractions of 13-18 Gy or 36-48 Gy in five to eight fractions. Treatment tends to be well tolerated with good efficacy. Due to the higher dose per fraction, side effects reported in the literature are brain necrosis, fistula formation and bleeding. [11-15]
The risks of re-irradiation include acute and chronic dysphagia, severe grade 3-4 mucositis, osteoradionecrosis, soft tissue necrosis, carotid rupture, fibrosis, long term tracheostomy and gastrostomy dependence and trismus. Treatment related mortality can be as high as 20% in some series. Favourable prognostic factors for overall survival, disease free survival and locoregional control are small T stage; no organ dysfunction; no patient co-morbidities; smaller tumour bulk after surgery; increased time since prior radiation; trimodality salvage and re-irradiation dose. Literature shows that improving locoregional control results in an improvement in overall survival. [7] The median re-irradiation doses vary between 60-66Gy in literature. In inoperable patients with small volume disease re-irradiation remains the only treatment option for cure.
In conclusion, there is a non-trivial cohort of patients with recurrence that can be salvaged. Trimodality therapy is associated with optimal outcomes. Re-irradiation is associated with substantial acute and late toxicities. Caregivers need to carefully balance risks and benefits of treatment and inaction. [7] Re-irradiation is a controversial topic which remains challenging especially for patients where other salvage treatment modalities are not an option. For the radiation oncologist it represents a fine balance between tumour related morbidity and treatment related toxicity.
Dr Nirasha Chiranjan
28 September 2017
- Vokes EE, Weichselbaum RR, Lippman SM, Hong WK: Head and neck cancer. N Eng J Med 1993, 328:184-94.
- Dawson LA, Anzai Y, Marsh L, Martel MK, Paulino A, Ship JA, Eisbruch A: Patterns of local-regional recurrence following parotid-sparing conformal and segmental intensity-modulated radiotherapy for head and neck cancer. Int J Radiat Oncol Biol Phys 2000, 6:1117-26.
- Kao J, Garofalo MC, Milano MT, Chmura SJ, Citron JR, Haraf DJ: Reirradiation of recurrent and second primary head and neck malignancies: a comprehensive review. Cancer Treat Rev 2003, 29:21-30.
- Kasperts N, Slotman BJ, Leemans CR, de Bree R, Doornaert P, Langendijk JA: Results of postoperative reirradiation for recurrent or second primary head and neck carcinoma. Cancer 2006, 106:1536-47.
- Mendenhall WM, Mendenhall CM, Malyapa RS, Palta JR, Mendenhall NP: Reirradiation of head and neck carcinoma. Am J Clin Oncol 2008,31:393-8.
- Kodani N, Yamazaki H, Tsubokura T, Shiomi H, Kobayashi K, Nishimura T, Aibe N, Ikeno H, Nishimura T: Stereotactic Body Radiation Therapy for Head and Neck Tumor: Disease Control and Morbidity Outcomes. J Radiat Res (Tokyo) 2011, 52:24-31.
- David J Sher: Dana-Faber Cancer Institute: Head and neck reirradiation: perils and practice
- Hepel JT, Syed AM, Puthawala A, Sharma A, Frankel P: Salvage high-doserate (HDR) brachytherapy for recurrent head-and-neck cancer. Int J Radiat Oncol Biol Phys 2005, 62:1444-50.23. Popovtzer A, Gluck I, Chepeha DB, Teknos TN
- Aird, E.G., Williams, J.R., Rembroska, A., “Brachytherapy”, Radiotherapy Physics in Practice, Oxford Univ. Press, Oxford (2000)
- Lee N, Chan K, Bekelman JE, Zhung J, Mechalakos J, Narayana A, Wolden S, Venkatraman ES, Pfister D, Kraus D, Shah J, Zelefsky MJ: Salvage reirradiation for recurrent head and neck cancer. Int J Radiat Oncol Biol Phys 2007, 68:731-40.
- Siddiqui F, Patel M, Khan M, McLean S, Dragovic J, Jin JY, Movsas B, Ryu S: Stereotactic body radiation therapy for primary, recurrent, and metastatic tumors in the head-and-neck region. Int J Radiat Oncol Biol Phys 2009, 74:1047-53.
- Himei K, Katsui K, Yoshida A, Takemoto M, Kobayashi M, Kuroda M, Sato K, Baba Y, Hiraki Y: Initial experiences of CyberKnife tratment for Head and Neck cancer. Head Neck Cancer 2002, 28:186-191
- Roh KW, Jang JS, Kim MS, Sun DI, Kim BS, Jung SL, Kang JH, Yoo EJ, Yoon SC, Jang HS, Chung SM, Kim YS: Fractionated stereotactic radiotherapy as reirradiation for locally recurrent head and neck cancer. Int J Radiat Oncol Biol Phys 2009, 74:1348-1455.
- Ogita M: Iamge guided radiotherapy (IGRT): Advancement and New technology of CyberKnife. Initial Experience. INNERVISION 2009, 24:63-65
- Heron DE, Ferris RL, Karamouzis M, Andrade RS, Deeb EL, Burton S, Gooding WE, Branstetter BF, Mountz JM, Johnson JT, Argiris A, Grandis JR, Lai SY: Stereotactic body radiotherapy for recurrent squamous cell carcinoma of the head and neck: results of a phase I dose-escalation trial. Int J Radiat Oncol Biol Phys 2009, 75:1493-1500.
 Apart from non-melanoma skin cancer, Breast Cancer is the most common cancer in women of all races, with a lifetime risk of 1 in 26 in South Africa, according to the 2012 National Cancer Registry (NCR). A large proportion of breast cancer patients receive adjuvant radiation therapy (RT) in either the breast conservation or the postmastectomy setting to improve locoregional recurrence rates and overall survival. Typically, patients requiring radiotherapy to the intact breast or chest wall with or without the regional nodal irradiation receive 4-6 weeks of treatment, the most common anticipated side effect is radiation dermatitis.
Apart from non-melanoma skin cancer, Breast Cancer is the most common cancer in women of all races, with a lifetime risk of 1 in 26 in South Africa, according to the 2012 National Cancer Registry (NCR). A large proportion of breast cancer patients receive adjuvant radiation therapy (RT) in either the breast conservation or the postmastectomy setting to improve locoregional recurrence rates and overall survival. Typically, patients requiring radiotherapy to the intact breast or chest wall with or without the regional nodal irradiation receive 4-6 weeks of treatment, the most common anticipated side effect is radiation dermatitis.
Pathophysiology of radiation dermatitis:
High-energy X-rays delivered during RT produce both direct and indirect ionization events that lead to damage of cellular macromolecules, most importantly in the form of double-stranded DNA breaks. Through this DNA damaging mechanism, RT affects all cellular types within the epidermis and dermis and leads to the clinical syndrome of radiation dermatitis.
Within the epidermis, radiation-induced DNA damage disrupts the normal proliferation and differentiation of basal keratinocytes. This results in the depletion if the differentiated epidermal keratinocytes and maintenance of this physical barrier is then lost.
Dermal radiation effects are much more complex. Sebaceous glands as well as hair follicles are acutely sensitive to low doses of radiation, resulting in acute skin dryness and hair loss. Microvascular injury within the dermis is responsible for both the acute as well as the chronic skin effects noted during radiotherapy. Of note “Proinflammatory cytokines and chemokines, such as interleukin (IL)-1, IL-6, IL-8, and tumor necrosis factor (TNF)-alpha, among others, have been found to play roles in immune cell activation, leukocyte transendothelial migration, and inflammatory oedema. Mast cell degranulation and histamine release also further the immune response and contribute to the clinical radiation dermatitis syndrome.” The effects of transforming growth factor (TGF)- beta on dermal fibroblasts are thought to contribute towards the late tissue fibrosis associated with radiotherapy
Presentation and Timing:
Radiation induced dermatitis develops in dose dependent, deterministic manner with predictable timing. Acute phase radiation dermatitis is defined as occurring typically within 30-90 days of radiation exposure.
Clinical symptoms of acute radiation dermatitis
| Skin reaction | Onset | Dose threshold (Gy) |
| Erythema | 7-10 days | 6-10 |
| Dry desquamation | 3-4 weeks | 20-25 |
| Moist desquamation | 4+ weeks | 30-40 |
| Ulceration | 5+ weeks | >40 |
The first clinically apparent skin change noted after breast irradiation is mild erythema. This is noted within hours of radiation exposure and presents as a faint and transient erythema. Most skin reactions are however noted within 10-14 days after initiation of radiotherapy and may progressively worsen throughout the remainder of the treatment. This skin reaction can include oedema, dryness of the skin, burning, itchiness, tenderness and hyperpigmentation. Also, common during this time is hyperpigmentation and sensitivity of the nipple areolar complex.
Dry desquamation typically occurs in doses in excess of 20Gy and clinically presents as peeling of dry skin and scaly skin which does not significantly add to patient morbidity. In contrast, wet desquamation is very painful due to the destruction and sloughing of dermal layers. It may also be associated with fluid drainage or “weeping” and is noticed after cumulative doses in excess of 30Gy. This often begins in small patches in skin folds and may progress to involve larger confluent areas typically in the axilla and the inframammary fold. Of note is that these symptoms peak in intensity approximately 1-2 weeks after the completion of radiotherapy.
Patient and treatment related risk factors:
Patient factors:
Breast cup size has consistently been shown to influence skin toxicity. A study from the Royal Marsden confirmed that patients with larger breast sizes were “five times more likely to experience acute skin reactions”. This finding was proven in many subsequent studies.
The body mass index (BMI) has also been shown to be an independent factor associated with moist desquamation. Since the worst skin reactions tend to occur in the inframammary fold and the axilla it is hypothesised that a greater self-blousing effect may the cause. The skin sparing effects of megavoltage radiation seems to be negated due to the build-up of skin on skin.
Other patient factors include:
- Degree of friction due to normal movement of the arm
- Types of clothing and texture
- Perspiration build up
Menopausal status and racial differences have been proven to be linked to radiation dermatitis risk. Post-menopausal patients as well as black patients have significantly higher rates if wet desquamation. Smoking effects have never conclusively been shown to contribute to worse acute radiation reactions.
Rare DNA mutation syndromes may also lead to severe acute radiosensitive, these include Ataxia-Telangiectasia, Nijmegen Breakage syndrome and Fanconi Anaemia
Treatment related factors:
The biggest change to the incidence of radiation dermatitis has to be the technological development of three-dimensional (3D) treatment planning. There is significant data to show that 3D planning techniques significantly decrease radiation induced skin reactions when compared to two-dimensional planning. Three dimensional techniques allow for changes in breast contour thereby reducing inherent radiation “hot-spots”.
Hypofractionation schedules are becoming increasingly more utilized. Hypofractionation implies delivery of a slightly higher daily dose of radiotherapy to an overall biologically equivalent total dose. The benefit of this dosing regimen is that it results in a shorter treatment time of 3-4 weeks instead of 5-6 weeks. Numerous prospective trials have consistently demonstrated similar long-term breast cancer outcomes using hypofractionation schedules compared to standard fractionation, without any increased toxicity. Data suggests that hypofractionation may show improved rates of dermatitis, pruritis, hyperpigmentation and breast pain in the acute setting.
Radiation dermatitis prevention: the evidence
Topical Steroids
There have been multiple prospective randomized trials that have shown that topical steroids are effective for diminishing radiation dermatitis. The “preventative effect of betamethasone on radiation dermatitis has been seen in both conventional and hypofractionated radiation settings”.
Non-steroidal Agents
Non-steroidal agents have consistently failed to show improvements in radiation dermatitis when compared prospectively. Multiple studies have shown that using Aloe Vera is ineffective in reducing acute skin reactions. A single study reported worse breast pain and dry desquamation in patients using Aloe Vera. Calendula ointment extracted from the Calendula officinalis plants has shown some promise when used a topical anti-inflammatory agent in wound healing.
Management of skin during breast radiotherapy
Skin washing:
Concerns that washing with soap and water may cause mechanical trauma have resulted in recommendations against washing in the radiation treatment fields. This theory was tested in a trial where patients were randomized to; no washing, washing with water alone or washing with soap and water. The patients who used soap and water were found to have significant reductions in “itching at the end of treatment and reduced erythema and desquamation scores 6-8 weeks following treatment”.
Current recommendations advise patients to wash skin daily with warm water and soap while avoiding scrubbing. A pH neutral soap is advised and the mildest of these is DOVE.
Deodorant and antiperspirant use:
Antiperspirants and deodorants were historically discouraged in breast cancer patients. It was felt that the metallic based formulations may increase skin reactions when interacting with radiation, as well as potentially creating a bolus like effect thereby increasing skin dose. Controlled studies have consistently found no evidence of worse skin outcomes with deodorant use when applied in standard thickness, changing the paradigm of prohibiting deodorant use during radiotherapy. Any enhanced skin reaction is related to the irritating chemical ingredients within the product itself and not “the metallic content or bolus effect”.
Barrier products for dermatitis treatment:
Cutaneous barriers are commonly used, to provide moisture and protect the skin form developing a secondary infection. Prospective comparisons have shown conflicting results and a standard treatment has yet to be identified. Numerous studies have compared hydrocolloid dressings to gentian violet and anti-microbial solution for open wounds, unfortunately no definitive answers are available.
Management of desquamation:
Dry desquamation is commonly associated with surface flaking of the stratum corneum. This is not in itself a cause for concern and the area should be well moisturized and kept clean and dry. Dry desquamation may progress to moist desquamation. It is important at this stage to document the size and location of the desquamation as well as the presence of an exudate. The recommended approach is to treat patient with saline soaks using normal saline compresses up to four times daily. The use of moisture retentive, barrier ointments after each soak is recommended.
Patients should be closely monitored for signs of infection such as fever, swelling, foul smelling purulent odour. Pain should be managed with analgesics based on the patient’s level of symptoms.
Conclusion
Despite our increasing awareness and understanding of the side effects of radiation treatment in breast cancer, radiation dermatitis continues to be among the most common side effects. In order to effectively manage patients with radiation dermatitis, one must be aware of the expected appearance and timing of symptoms, the appropriate scoring systems for properly monitoring symptom severity over time, and should follow evidence-based guidelines for treatment when
possible.
Kole A,Kole L,Moran M.S. Acute Radiation dermatitis in breast cancer patients: challenges and solutions. Breast cancer – Targets and Therapy. 2017:9 313-323.
Dr Marlene Soares
28 September 2017
 Lung Cancer
Lung Cancer
is the most common cancer worldwide, and also the greatest cause of cancer-related deaths. Through the course of the twentieth century the incidence of lung cancer increased steadily, but due to improved public awareness and fewer people smoking, the number of cancer related deaths have started to decline.
Screening
The National Lung Screening Trial in the USA compared CT screening with CXR in patients who are at risk of developing lung cancer. In this trial, CT-screened individuals showed a 20% reduction in lung cancer mortality compared to those screened with CXR only. This trial identified the ideal candidates for screening as asymptomatic patients between 55 and 77 years, who have a smoking history of at least 30 pack-years, and (if not smoking any longer) have not quit smoking more than 15 years before screening starts.
Pathology
Up until about a decade ago, the clinician based treatment decisions on TNM stage and whether the tumour was a small-cell (SCLC) – roughly 15% of all lung cancer – or non-small-cell lung cancer (NSCLC). For NSCLC, we now know that there is an important difference between adenocarcinoma (about 45%) and squamous cell carcinoma, and as such patients with stage IV NSCLC receive different treatments. Routine analysis to identify specific mutations (including epidermal growth factor receptors(EGFR) and anaplastic lymphoma kinase (ALK) receptors in adenocarcinoma) for which targeted therapies are available, make it possible to tailor patients’ treatment and optimize responses.
Treatment
General
A very brief outline of general guidelines will follow. Exciting new developments in the fields of targeted and immune therapy in recent years give hope of improving the low survival rate (around 15% at five years) for stage IV disease, but however are out of the scope of this article.
Stage I and II
These are ideally treated surgically. The preferred procedure is a lobectomy with lymph node dissection of the unilateral mediastinal nodes. For pathological stage II and some IB tumours, adjuvant chemotherapy is indicated. Radiation therapy reduces local recurrences where margins are involved microscopically. When lymph node metastases are found (pathologic stage III), adjuvant chemotherapy followed by radiation is indicated.
For patients who are unfit for surgery, radiation therapy is an alternative treatment. Stereotactic body radiotherapy (SBRT) can deliver a few high doses of radiation to a precisely localized target, resulting in a highly effective ablative treatment. Where this technology is not available, more conventional methods of external beam radiotherapy (RT) are used commonly with satisfactory results.
”At DMO, we have stereotactic body radiotherapy treatment available at both our Sandton Oncology and Groenkloof Radiation Oncology units.”
Comparisons with historic data show that conventional RT yields inferior survival rates compared to surgery (30-50% vs. 50-70% for stage I at 5 years). To date no head-to-head comparisons are available to compare SBRT and surgery, and even though SBRT is superior to RT, surgery should still be the treatment of choice for operable stage I and II patients.
Stage III
Stage III disease is defined as either a locally advanced tumour (T3 and T4), and/or patients with mediastinal lymph nodes, in the absence of metastases. This is a heterogeneous group of patients, and the fact that staging systems have changed over the years make it difficult to extrapolate historical data to make treatment decisions. International guidelines are available to assist clinicians in the management of patients.
One of the most critical steps in devising a management plan for the stage III patient is accurate nodal staging. This is a particularly involved process, and should ideally be carried out by a surgeon with experience in lung cancer management. Imaging is used as a starting point to determine the exact surgical work-up a patient will need, as some stage III patients may still be candidates for radical surgery.
Concurrent chemo-radiotherapy is the treatment of choice for most patients who are not surgical candidates. These patients receive a platinum-based regimen and standard dose RT. This approach has been shown to achieve better survival compared to sequential treatment (chemo followed by RT). For patients who are not medically fit to tolerate chemotherapy, RT can offer effective palliation of symptoms and a modest improvement in survival.
Stage IV
Patients with advanced, metastatic lung cancer are considered incurable and unfortunately have a poor prognosis. The aim of treatment is to prolong life if possible, address symptoms due to the disease, maintain a good quality of life and limit the adverse effects caused by treatment.
The following factors are considered when devising a treatment strategy:
- The disease burden – how many sites of metastases are present and how symptomatic the patient is
- Histologic type – squamous vs. adenocarcinoma
- Molecular findings – the presence of mutations such as EGFR and ALK
- Programmed death ligand 1 (PDL-1) expression (high)
After progression on one line of treatment, several further options are available depending on initial therapy and above-mentioned factors.
Radiation therapy can be of benefit to stage IV patients in the following situations:
- Limited metastases (oligometastatic): SBRT can offer effective control of a single area of recurrence or metastasis.
- Bone metastases: RT is highly effective to relieve pain caused by bone metastases.
- Brain metastases: Whole brain radiotherapy can offer patients relief from headache, nausea, and pressure effects of intracranial tumours, but is often associated with long-term cognitive decline. In the case of few brain metastases as well as good control of the local lung tumour and no other spread, stereotactic radiotherapy can be used to treat the brain lesion(s) only and spare the patient the effects of whole brain irradiation.
Surveillance
Follow-up is crucial both in successfully treated localized tumours as well as patients with metastatic disease. In case of the former, early detection of recurrence can allow for more effective salvage therapy, and to start earlier with systemic therapy for metastatic disease can potentially prolong a patient’s life. In case of the latter, it is beneficial to start with alternative systemic therapy as soon as progressive disease is evident.
Patients come for follow-up visits and CXR every three months and an annual CT scan. PET-CT can also be considered. After two years less frequent follow-up (6-monthly) is sufficient. When patients exhibit clinical symptoms and signs of bone or lung metastases, a bone scan or brain CT scan is appropriate.
Conclusion
- Lung cancer is a common malignancy, with personal or second-hand smoke being a major risk factor. The primary care doctor should discourage youngsters to start and encourage smokers to stop smoking as a preventative strategy.
- For patients who have a strong smoking history and are asymptomatic, screening CT scan of the chest should be considered.
- The best outcomes are in patients with stage I and II disease who are able to undergo curative surgery and adjuvant therapy as indicated.
- For most stage III patients combined chemo-radiotherapy is the preferred treatment strategy.
- Radiation therapy is an effective alternative for patients who are medically unfit for surgery and/or chemotherapy. Stereotactic body radiotherapy can offer high doses of precisely localized radiation to selected tumours.
- Stage IV patients are considered incurable and the aim of treatment is to maintain quality of and limit treatment side-effects. In many cases treatment may also provide longer survival to patients.
- Radiotherapy can offer durable and effective palliation of bone metastases.
- Brain metastases can benefit from radiotherapy to improve symptoms of headache and obstruction.
- In the case of limited brain-only lesions, stereotactic radiotherapy can spare patients from cognitive decline while still controlling the tumour.
Sources:
- UpToDate website
- Handbook of Evidence-Based Radiation Oncology, 2nd edition; Eric K. Hansen and Mark Roach III (editors)
Dr Maryke Etsebeth
22 September 2017
According to the latest National Cancer Registry (NCR 2012), the number of cases diagnosed in that year was 6807.
The estimated life time risk is 1:19 and makes-up 18,45% of all cancers diagnosed,” said specialist radiation oncologist, Sudeshen Naidoo. The median age of diagnosis is 70 years, but with increased screening, more younger men are being diagnosed. The prostate gland consists of the peripheral zone (70% of glandular prostate and site of nearly all cancers), the central zone (25% of the glandular prostate), the transition zone (surrounding the urethra and the site of benign prostatic hypertrophy), and the anterior fibromuscular stroma. “Approximately 50-80% of tumours involve the prostate apex, and around 85% of patients have multifocal disease in the prostate. More than 95% of prostate cancers are adenocarcinomas,” said Naidoo. Potential risk factors » Advanced age » Benign prostatic hypertrophy » Diet e.g. high-fat intake » Family history of prostate cancer – frequency of prostate cancer, increases with family history of first degree relatives with prostate cancer. » Hormonal factors e.g serum testosterone and androgens are required for the development of prostate cancer » Race /ethnicity e.g Black.
DSTV, ITV – Let’s Talk – Breast Cancer and the Pink Drive initiative
1 in 29 people will be diagnosed with breast cancer in South Africa, says Specialist Radiation Oncologist Dr Sudeshen Naidoo.
At least 6 849 cases of female breast cancer are diagnosed annually, he explains.
But Dr Naidoo advises that men are also at risk of having breast cancer, although the statistics are much lower.
He explores the common risk factors associated with breast cancer such as age and child birth.
Take a listen:
Written by: Qama Qukula
702 welcomes all comments that are constructive, contribute to discussions in a meaningful manner and take stories forward.
However, we will NOT condone the following:
- Racism (including offensive comments based on ethnicity and nationality)
- Sexism
- Homophobia
- Religious intolerance
- Cyber bullying
- Hate speech
- Derogatory language
- Comments inciting violence.
We ask that your comments remain relevant to the articles they appear on and do not include general banter or conversation as this dilutes the effectiveness of the comments section.
We strive to make the 702 community a safe and welcoming space for all.
702 reserves the right to: 1) remove any comments that do not follow the above guidelines; and, 2) ban users who repeatedly infringe the rules.
Should you find any comments upsetting or offensive you can also flag them and we will assess it against our guidelines.
702 is constantly reviewing its comments policy in order to create an environment conducive to constructive conversations.
Latest Posts
Article Categories
A DMO Centre Near You
| Ahmed Kathrada Cancer Institute Ahmed Kathrada Private Hospital K43 Highway Lenasia Extension 8 Johannesburg, Gauteng +27 (10) 900 3199 View Map |
Sandton Oncology 200 Rivonia Medical Centre 200 Rivonia Road Morningside, Sandton +27 (11) 883 0900 View Map |
West Rand Oncology Centre Flora Clinic Cnr William Nicol Road & Joseph Lister Avenue Floracliffe, Roodepoort +27 (11) 991 3500 View Map |
Muelmed Radiation Oncology Muelmed Hospital 577 Pretorius Street Arcadia, Pretoria +27 (12) 440 8089 View Map |
Groenkloof Radiation Oncology Life Groenkloof Hospital 50 George Storrar Dr Groenkloof, Pretoria +27 (12) 460 4749 View Map |
© De Mûelenaere Oncology 2018.